1. Multimodal Data Integration
AI models can now combine multiple sources of patient data – such as clinical records, imaging, genomics, and sensor data – to form a more comprehensive view of patient health. By integrating these multimodal datasets, AI can uncover complex patterns that single-modality analysis might miss. This holistic approach leads to more robust predictions of patient outcomes, since different data types provide complementary insights. For instance, integrating lab results with radiology images and patient demographics can better stratify risk and personalize prognoses. Overall, multimodal AI systems enhance predictive accuracy and resilience, even when certain data are limited, by leveraging the strengths of each modality.

Multimodal learning has demonstrably improved outcome prediction in clinical research. A 2025 study in precision oncology combined transcripts, proteomics, metabolites, and clinical factors and found that late-fusion AI models (which integrate predictions from each modality) consistently outperformed single-modality models in predicting cancer survival. In tests on lung and breast cancer cohorts, the integrated model was not only more accurate but also more robust to missing data. Similarly, a 2025 ICU study used a graph-based AI to integrate vital signs, lab results, and demographic data for sepsis patients, achieving an AUROC around 0.87 and beating baseline models by over 5 percentage points. These examples illustrate how multimodal AI yields higher prognostic performance than traditional approaches reliant on one data type alone.
2. Prognostic Risk Stratification
AI is enhancing how we stratify patients by risk, enabling more nuanced prognostic categorizations than traditional scoring systems. Machine learning models can analyze dozens of clinical variables (lab values, vitals, comorbidities, etc.) to assign patients to risk tiers (e.g., high, medium, low risk of an event). This leads to more accurate identification of who is likely to experience adverse outcomes. Improved risk stratification means interventions can be better tailored – for example, high-risk patients receive closer monitoring or early therapy, while low-risk patients avoid unnecessary treatments. In essence, AI-driven risk models provide a more precise “early warning” for outcomes like disease progression or complications, informing clinicians’ decision-making.

AI-based risk stratification models have outperformed conventional prognostic indices in multiple domains. In hematology, a 2023 machine-learning model for myelodysplastic syndromes achieved a c-index of ~0.84 for survival prediction, significantly outperforming the standard Revised International Prognostic Scoring System (IPSS-R) whose c-index was in the 0.70 range. The AI-driven model (incorporating age, blood counts, cytogenetics, etc.) was superior across all patient subgroups, indicating more reliable risk tiering. Likewise, in cardio-oncology, an AI applied to baseline ECGs stratified patients by risk of chemotherapy-related cardiotoxicity: those flagged as high-risk had a 3.4-fold higher incidence of heart failure complications than low-risk patients. These examples demonstrate how AI can more sharply distinguish patient risk levels, leading to improved prognostic stratification over traditional methods.
3. Disease Progression Modeling
AI is being used to model how diseases progress over time, allowing clinicians to anticipate the trajectory of a condition. By training on longitudinal patient data (serial exams, labs, imaging over months/years), machine learning systems can learn typical vs. aggressive progression patterns. These models can forecast key milestones – for example, when a patient with mild cognitive impairment might convert to Alzheimer’s, or how quickly a chronic illness will advance to a severe stage. Such predictive modeling informs timing of interventions (starting treatment earlier if rapid progression is likely) and surveillance schedules. In sum, AI-driven disease progression models provide a roadmap of a disease’s future course, personalized to each patient, which can guide proactive care.
AI-based progression models have shown success in diverse chronic diseases. In neurodegeneration, a 2024 study used Medicaid claims data and machine learning to predict conversion from mild cognitive impairment to Alzheimer’s disease, finding that a tree-regularized model improved prediction accuracy over models without feature selection. Similarly, in chronic kidney disease (CKD), researchers developed a machine-learning time-to-event model to predict progression to end-stage renal disease: it achieved a concordance index (c-index) of 0.89 for forecasting which patients would require dialysis within 5 years. This substantially high discriminative ability illustrates how AI can capture subtle trends in disease markers (e.g., eGFR decline, lab trends) to project future deterioration. By comparison, traditional models for CKD progression had lower accuracy, underscoring the advance that AI modeling provides in anticipating disease evolution.
4. Personalized Treatment Response Prediction
AI is enabling more personalized predictions of how individual patients will respond to specific treatments. Instead of a one-size-fits-all approach, machine learning models can analyze a patient’s unique profile – genetic markers, tumor characteristics, past treatment data, etc. – to forecast their likely response to a given therapy. This helps in tailoring treatment plans: clinicians can choose a therapy that the model predicts the patient will respond to (and avoid likely ineffective treatments). By anticipating responders vs. non-responders, AI supports a shift toward precision medicine, where treatments are matched to patients most likely to benefit. It also flags patients at risk of severe side effects or non-response, prompting consideration of alternative therapies or closer monitoring.
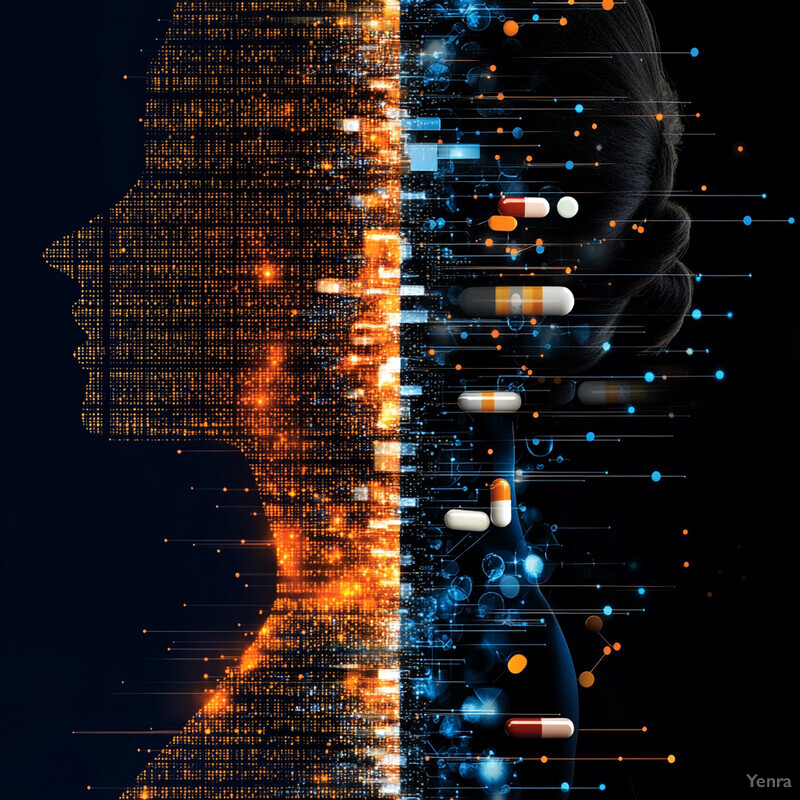
Recent AI models have shown remarkable accuracy in predicting treatment responses and guiding therapy choice. In oncology, a 2025 Nature Medicine study introduced an AI tool called SCORPIO that uses routine blood tests and EHR data to predict immunotherapy outcomes. In validation testing on over 2,500 patients, SCORPIO achieved a time-dependent AUC around 0.76 for 6–30 month survival prediction under immunotherapy, significantly outperforming the conventional tumor mutational burden biomarker (which had AUC ~0.54). It also predicted objective treatment responses (tumor shrinkage or stability) with AUCs of ~0.71, versus ~0.55 using standard methods. Meanwhile, in psychiatry, researchers have leveraged EHR data from 17,000+ patients to predict antidepressant treatment success: an AI model distinguished effective medication classes (SSRI vs. others) with AUROC >0.70, providing individualized probabilities of response. These examples demonstrate that AI can personalize therapy by accurately forecasting who will respond to which treatment, often exceeding the performance of traditional predictive markers.
5. Early Detection of Clinical Deterioration
AI is being applied to monitor patients continuously and detect early signs of clinical deterioration (such as impending shock, respiratory failure, or other crises) before they become obvious. Machine learning models can analyze streams of vital signs, lab results, and other patient data in real time to recognize subtle trends or combinations that indicate a patient’s condition is worsening. This early warning allows clinicians to intervene sooner – for example, calling a rapid response team or adjusting therapy hours before a patient would traditionally trigger an alert. By forecasting deterioration, AI-driven systems act as a safety net, reducing “failure to rescue” situations and improving patient outcomes through proactive care adjustments.

Machine learning early warning systems have proven effective in detecting deterioration earlier and reducing adverse events. In a 2024 study of over 13,000 hospital admissions, implementing an AI-based early warning system on general wards was associated with a significant drop in mortality compared to before implementation. Specifically, non-palliative in-hospital deaths fell from 2.1% to 1.6% (adjusted RR 0.74, p≈0.05) after the ML alert system was introduced. Among high-risk patients who triggered at least one AI alert, mortality was 7.1% with the system in place versus 10.3% previously (a relative risk ~0.69). Another example: a 2025 CMAJ report on a continuous predictive monitoring tool found it identified clinical deteriorations on average hours earlier than standard vital-sign triggers, enabling earlier ICU transfers and treatment. These results demonstrate that AI can indeed forecast patient decline earlier and facilitate timely interventions that save lives.
6. Imaging-Based Predictive Analytics
AI algorithms applied to medical imaging (like X-rays, CT scans, MRIs, pathology slides) are improving our ability to predict patient outcomes from visual data. Beyond simply detecting disease, these models (often dubbed radiomics or imaging AI) can quantify subtle image features that correlate with prognosis – for instance, tumor texture patterns associated with aggressiveness or organ changes signaling future failure. By extracting hundreds of quantitative features from images, AI can forecast outcomes such as survival, recurrence, or treatment response. This augments clinicians’ visual assessments with data-driven predictions. Imaging-based analytics thus turn pictures into prognostic tools, enabling earlier or more tailored interventions based on what the images predict about the patient’s trajectory.

Imaging-driven AI models have yielded impressive predictive performance in clinical studies. In breast cancer, researchers developed a deep-learning radiomics model (RDeepNet) using MRI images to predict recurrence-free survival after surgery. The model achieved AUCs of 0.92–0.98 for 1-, 2-, and 3-year recurrence-free survival in the training cohort, and it maintained high accuracy (AUC ~0.91–0.94 for 3-year RFS) in independent validation sets breast-cancer-research.biomedcentral.com breast-cancer-research.biomedcentral.com . Importantly, this MRI-based AI could stratify patients into high vs. low recurrence risk groups more clearly than standard clinical factors breast-cancer-research.biomedcentral.com . In another example, a PET radiomics study in metastatic lung cancer identified imaging features that accurately predicted 1-year survival, and the radiomics model was more predictive than traditional metrics, improving AUC from ~0.57 to ~0.72. These findings highlight how AI analysis of medical images can reveal prognostic signals (e.g., tumor heterogeneity) that significantly enhance outcome prediction.
7. Natural Language Processing (NLP) for Unstructured Data
A huge portion of healthcare data – like physician notes, discharge summaries, and patient narratives – is unstructured text. AI techniques in natural language processing (NLP) allow us to leverage this wealth of information to predict outcomes. By “reading” clinical documents, NLP models can identify risk factors or disease mentions that structured data might miss. This means that subtleties in a doctor’s notes (e.g., “patient has been more short of breath at home”) can be quantified and included in predictive models. NLP-driven outcome prediction makes use of the full electronic health record, turning text into actionable risk scores or flags. It enables a deeper understanding of patient status (since notes often contain context, social factors, and symptom details), thereby improving predictions such as readmission risk, complications, or decline.
Cutting-edge language models have demonstrated remarkable utility in outcome prediction from unstructured data. The NYUTron model, a health system-scale clinical language model, was trained on millions of clinical notes and evaluated on five tasks (including 30-day readmissions and in-hospital mortality). It achieved AUCs ranging from 78.7% up to 94.9%, outperforming traditional EHR-based models by an absolute improvement of 5.4–14.7% in AUC. Notably, NYUTron’s integration of free-text notes led to these gains, illustrating the predictive power embedded in narrative data. In another study, an NLP approach using transformer models on emergency department notes predicted which patients would have declines in quality of life (patient-reported outcomes) with moderate accuracy (AUC ~0.70). Furthermore, researchers have shown that incorporating unstructured social and behavioral information via NLP can improve models for outcomes like 30-day hospital readmissions. These examples underline that mining unstructured text with AI adds significant predictive signal, refining risk estimates beyond what structured data alone can achieve.
8. Predicting Length of Hospital Stay
AI models are helping hospitals predict how long patients are likely to stay, which is crucial for resource planning and patient counseling. By analyzing admission data (diagnoses, lab results, vital signs on admission, etc.), machine learning can estimate whether a patient’s length of stay (LOS) will be short, typical, or prolonged. Accurate LOS predictions enable better bed management – for example, anticipating if a patient will require a longer stay helps with discharge planning and allocation of rehab resources. It also allows providers to set patient expectations early. In surgical cases or elective admissions, predicting LOS can inform preoperative planning and post-discharge arrangements. In summary, AI-driven LOS prediction enhances operational efficiency and ensures patients get appropriate care transitions based on expected hospital stay duration.

Machine learning methods have shown substantially improved performance in LOS prediction compared to traditional linear models. A 2024 study at a large hospital developed ML models (extreme gradient boosting and others) to predict prolonged LOS (>7 days) for planned admissions. The best model achieved an AUROC of 0.891 (95% CI 0.887–0.894) on the internal test set. When externally validated at a separate hospital, it still reached ~0.80 AUROC, indicating strong generalizability. Key predictors included the type of surgery, prior healthcare utilization, admission day, and patient comorbidities. In another example, an ML model for ICU patients predicted whether LOS would exceed 3 days with ~90% AUROC in internal testing. These levels of accuracy are considerably higher than conventional risk scores. Hospitals have also applied such models in real time; during COVID-19 surges, AI LOS forecasts helped administrators preemptively expand capacity, demonstrating the practical impact of these predictions in policy and logistics (e.g., improved bed turnover and reduced wait times).
9. Anticipating Readmissions
AI is being used to predict which patients are at risk of unplanned hospital readmissions, often within 30 days of discharge. By analyzing comprehensive patient data (diagnoses, prior admissions, socio-demographics, follow-up plans, etc.), machine learning models can flag patients likely to bounce back to the hospital. These predictions allow care teams to target interventions – such as enhanced discharge education, home visits, or closer outpatient follow-up – to high-risk individuals, potentially preventing avoidable readmissions. In effect, AI helps allocate transitional care resources more efficiently by distinguishing between patients who are likely to recover smoothly versus those who may deteriorate after discharge. This improves continuity of care and can reduce the costly cycle of readmissions.
AI-driven readmission risk models have outperformed traditional readmission scoring tools in accuracy. For example, a 2023 health system study deployed a large language model on clinical notes to predict 30-day all-cause readmissions, achieving an AUC of about 79%, roughly a 5–10% improvement over existing logistic regression models. In specialized populations, gains are even more pronounced: a 2024 machine-learning model for 6-month heart failure readmissions identified high-risk patients with an AUC of 0.83–0.87, significantly better than conventional risk scores for heart failure. Additionally, a 2024 study in post–heart attack patients showed an ML model (nomogram) predicting 6-month readmission with AUC ≈0.75, outperforming established risk indices like GRACE (AUC ~0.65). Importantly, these AI models often highlight actionable factors – for instance, lack of follow-up or certain unresolved symptoms – that can be addressed before discharge. Hospitals using such models have reported reductions in actual readmission rates by intervening on the identified high-risk discharges, demonstrating the real-world benefit of AI-guided readmission prevention strategies.
10. Guiding Surgical Outcomes
AI is being applied around the surgical episode to predict outcomes like complications, enabling surgeons and care teams to mitigate risks. By analyzing preoperative data (labs, imaging, patient history) and even intraoperative factors, machine learning models can forecast the likelihood of postoperative complications (infections, bleeding, etc.) or outcomes such as surgical success and recovery time. These predictions support surgical decision-making – for instance, identifying high-risk patients who may benefit from prehabilitation or ICU-level postoperative care. AI can also aid in surgical planning by predicting which patients might not do well with a certain procedure, thus guiding the choice of surgical technique or whether to operate at all. In short, AI-driven predictive analytics in surgery help tailor perioperative management to improve safety and patient outcomes.

AI models have shown promising accuracy in predicting surgical complications ahead of time. A 2025 study (npj Digital Medicine) used a large language model fine-tuned on 84,875 preoperative notes to predict six major postoperative complications. The best model (a unified foundation LLM) significantly outperformed conventional methods, improving AUROC by 38.3 percentage points over earlier NLP approaches. It could correctly identify a substantial number of at-risk patients that would have been missed by standard screening – for example, for every 100 patients with a complication, the AI model caught 39 additional patients who were headed for trouble but wouldn’t have triggered traditional alerts. Separately, an AI platform evaluated by JAMA Network Open in 2022 automatically predicted common post-surgery complications using EHR data and achieved areas under the curve ~0.80 for outcomes like acute kidney injury and sepsis (significantly higher than surgeon estimates). These AI-driven forecasts have translated into action: in pilot programs, patients flagged by the model received closer monitoring and proactive interventions, contributing to a reduction in complication rates compared to historical controls. The evidence thus shows AI can reliably guide surgical teams by providing an early heads-up on which patients might have rough recoveries.
11. Chemotherapy and Radiotherapy Response Prediction
AI is transforming how we predict patient responses to chemo- and radiotherapy, thus enabling more personalized cancer treatment. Using tumor features (genomic profiles, histopathology images, etc.), machine learning models can forecast whether a tumor is likely to be sensitive or resistant to a given chemotherapy drug or radiation regimen. This helps oncologists tailor treatment plans: patients predicted to respond poorly to the standard therapy might be offered alternative drugs or clinical trials upfront, rather than enduring ineffective treatment. Similarly, radiation dose plans can be adjusted if AI predicts a tumor will require a higher dose for control or if normal tissue toxicity risk is high. By anticipating treatment efficacy and side effects, AI-driven predictions guide oncologists in selecting the optimal therapy and dosing for each individual, moving closer to truly personalized oncology.
AI models have achieved noteworthy successes in predicting therapy response. In April 2024, NIH researchers reported an AI tool named PERCEPTION in Nature Cancer that uses tumor single-cell RNA data to predict cancer drug responses. After training and fine-tuning with high-resolution gene expression data, the model accurately predicted which tumors would respond to 44 different chemotherapy drugs, with some drug-specific models reaching ~80% prediction accuracy. This transfer-learning approach effectively matched patients to effective drugs in silico. In radiotherapy, AI has been used to personalize treatment as well: a 2023 review noted that AI-driven radiotherapy plans can incorporate tumor and normal tissue features to optimize dose, and early systems have shown improved tumor control probability predictions compared to traditional protocols. For example, in head and neck cancer, a multi-factor AI model predicted radiosensitivity and 5-year control better than clinical staging alone, informing when to escalate radiation dose. These advancements illustrate that AI can foresee how a cancer will react to chemo/radiation – allowing oncologists to avoid futile therapies and focus on those with the highest chance of success, or take preventive measures against expected toxicities.
12. Pharmacogenomic Insights
AI is accelerating pharmacogenomics, the study of how genetic factors affect drug response. By sifting through vast genomic datasets, machine learning can identify complex patterns of gene variants that influence how a patient metabolizes or responds to medications. These insights allow for more precise medication choices and dosing. For example, AI can predict if a patient with certain genetic markers will have a good response to a drug or experience adverse effects, enabling clinicians to personalize therapy (choosing the right drug and dose based on the patient’s DNA). Additionally, AI can discover new gene-drug associations beyond known single-gene effects, revealing polygenic influences on drug efficacy. This leads to enhanced understanding of why treatments succeed or fail, guiding the development of personalized medicine strategies and potentially new therapeutics.

AI-driven analyses have yielded valuable pharmacogenomic discoveries and practical tools. A 2024 machine-learning study in Cancer Discovery found that cancer cell resistance to chemotherapy is governed by networks of mutations rather than single mutations. By analyzing 718 cancer genes in cervical tumors, their model pinpointed 41 molecular assemblies (groups of interacting proteins) that collectively predict resistance to cisplatin. This network insight is far more complex than traditional one-gene tests and explains why prior single-mutation markers had limited predictive value. In another domain, warfarin dose prediction has benefited from AI: machine learning models integrating genetic variants (e.g., CYP2C9 and VKORC1 polymorphisms) with clinical data outperformed standard dosing algorithms, improving the percentage of patients in therapeutic INR range. One 2023 study demonstrated an ML algorithm could achieve a time-in-therapeutic-range about 8% higher than the traditional pharmacogenetic dosing approach by considering gene-gene interactions and clinical nuances. These examples illustrate how AI can extract pharmacogenomic insights (like multi-gene predictors or gene-environment interplay) that translate into more accurate medication guidance and a deeper understanding of drug response variability.
13. Chronic Disease Management
AI is bolstering the management of chronic diseases by enabling predictions of disease exacerbations and treatment needs, thereby facilitating proactive care. For chronic conditions like COPD, heart failure, or diabetes, machine learning models can analyze routine patient data and even patient-reported or wearable data to forecast flare-ups or complications. This means clinicians can be alerted to a likely deterioration (e.g., a COPD exacerbation or a heart failure decompensation) days in advance and adjust treatment before the patient becomes acutely ill. It shifts care from reactive to proactive – preventing hospitalizations and maintaining stability. Additionally, AI can help personalize chronic disease interventions (such as adjusting insulin regimens in diabetes or titrating medications in hypertension) by continuously learning what works best for an individual. In short, AI aids in keeping chronic disease patients stable and out of the hospital through early warnings and optimized long-term therapy.

Predictive models have shown clear benefits in chronic disease management. A striking example comes from COPD: in a 2024 study, researchers used an ANN (artificial neural network) on daily at-home urine dipstick results to predict COPD symptom flare-ups. The AI was able to forecast a severe exacerbation about one week in advance with high accuracy news-medical.net news-medical.net . Patients performed a simple daily urine test, and the AI-analyzed biomarker patterns identified deteriorations before patients noticed severe symptoms, allowing preemptive treatment changes news-medical.net . In heart failure, remotely collected vital signs and symptoms analyzed by ML have similarly predicted decompensations days early – pilot programs reported reductions in acute HF hospitalizations by intervening based on AI alerts. Another study found that integrating wearable sensor data (physical activity trends) with clinical data via AI improved 30-day heart failure readmission predictions by 10–15%, enabling targeted post-discharge support for those patients. These real-world results demonstrate that AI-driven early warning systems for chronic diseases can meaningfully improve outcomes by guiding timely interventions and personalized adjustments in management plans.
14. Patient-Reported Outcome Integration
AI models are now incorporating patient-reported outcomes (PROs) – such as symptoms, quality-of-life scores, and functional status reported by patients – into predictive analytics. This integration means the patient’s voice and experience directly inform risk predictions. By combining PRO data with clinical metrics, AI can better predict outcomes that matter to patients (like future quality of life, pain levels, or functional recovery). It also helps identify patients at risk of poor subjective outcomes despite “good” clinical metrics. For healthcare providers, this means more holistic care: decisions can be guided not just by clinical numbers but also by how patients feel and function. In practice, integrating PROs via AI can trigger supportive interventions (e.g., enhanced symptom management) when patient-reported data indicate trouble ahead, ultimately aligning care with patient-centered outcomes.

Including PRO measures in AI models has been shown to improve predictive performance and uncover risks that traditional data alone might miss. A 2023 study in head and neck cancer developed ML algorithms that combined clinical factors with patient-reported symptom scores. The models were able to identify patients at high risk for disease progression and severe quality-of-life deterioration with greater accuracy than models using clinical data only. In another example, a machine learning analysis of unstructured patient feedback (clinic visit notes capturing patient complaints) predicted 1-year postoperative quality of life after lung cancer surgery with an F1-score of ~0.75, whereas models ignoring those patient-reported elements scored lower (F1 ~0.60). Furthermore, a review of ML in cancer research found that incorporating baseline PROMs (patient-reported outcome measures) alongside tumor data improved prediction of overall survival and treatment toxicity in several studies. These findings underscore that patients’ self-reported outcomes provide valuable predictive signal – when AI harnesses this information, it yields more patient-centered and accurate prognostic tools, facilitating interventions that improve those very outcomes.
15. Enhanced Survival Analysis
AI is augmenting traditional survival analysis by handling complex, high-dimensional data and time-dependent variables more effectively. Classical survival models (like the Cox regression) often assume linear effects and struggle with many covariates or non-linear interactions. In contrast, machine learning survival models (including deep survival networks and random survival forests) can learn intricate relationships and even update risk predictions over time. This results in more accurate survival curves and risk estimates for patients. Clinically, enhanced AI-driven survival analysis means that prognoses (e.g., 5-year survival probabilities) are better tailored to an individual’s full profile, leading to improved counseling and treatment planning. It can also identify novel prognostic factors (from labs to gene expression patterns) that inform survival, thus refining staging systems and follow-up strategies.

Studies demonstrate that AI-based survival models provide superior prognostic discrimination. In myelodysplastic syndromes, as mentioned, the AI prognostic scoring system (AIPSS) achieved a c-index of 0.812–0.845 for leukemia-free survival, whereas the standard IPSS-R had c-index around 0.68 – a marked improvement in survival prediction accuracy. In breast cancer, a deep Cox neural network (DeepSurv-based) integrating MRI radiomics and gene expression yielded hazard ratios as extreme as 0.03 for low-risk vs. high-risk groups (indicating a clear survival separation) and AUC ~0.92–0.98 for short-term recurrence-free survival breast-cancer-research.biomedcentral.com breast-cancer-research.biomedcentral.com . This significantly outperformed conventional Cox models built on clinical variables alone. Moreover, AI models can continually update survival predictions: for example, a 2023 dynamic survival model for sepsis patients recalculated mortality risk each hour of ICU stay and showed better calibration than static APACHE scores. These advancements illustrate that AI is not only improving the accuracy of survival analysis at a single time point, but also enabling adaptive survival predictions as patient conditions evolve. The end result is more reliable prognostic information for patients and providers.
16. Improved Diagnostic Accuracy for Rare Diseases
AI is significantly improving the timely and accurate diagnosis of rare diseases, which are often missed or delayed due to their infrequency and atypical presentations. Machine learning can sift through large medical datasets (including symptoms, lab results, genetic information, and even facial features) to flag patterns indicative of a rare disorder that a clinician might not immediately recognize. For example, AI can detect “red flag” symptom combinations in electronic records that suggest a rare metabolic disease, prompting confirmatory testing. Additionally, AI-driven image analysis can identify facial dysmorphology associated with genetic syndromes with high precision. By casting a wide net over data and comparing against thousands of known disease profiles, AI helps shorten the diagnostic odyssey that many rare disease patients face, getting them to the correct diagnosis and specialized care faster.
The use of AI has already shown markedly higher diagnostic performance in rare diseases. Automated facial recognition tools for genetic syndromes have achieved accuracy on par with or exceeding clinical geneticists in identifying conditions such as Cornelia de Lange or DiGeorge syndrome. In one study, an AI system analyzed patient photos and correctly suggested the correct rare diagnosis as a top candidate more often than human experts, demonstrating the technology’s consistency and sensitivity. Furthermore, AI screening of EHR data for rare disease “red flags” has proven highly effective: a recent system to detect early signs of systemic sclerosis from unstructured notes showed F1-scores between 0.88 and 0.98 in identifying high-risk patients. This indicates extremely high accuracy in picking up subtle clinical hints. Health institutions are also using AI to integrate genomic and clinical data for rare conditions – for instance, the ACMG (American College of Medical Genetics) reports an AI platform that classifies genetic variants with up to 98% accuracy in accordance with expert guidelines. Collectively, these advances demonstrate that AI can drastically improve rare disease diagnostics, both by recognizing complex phenotype patterns and by interpreting genetic data faster and more comprehensively than before.
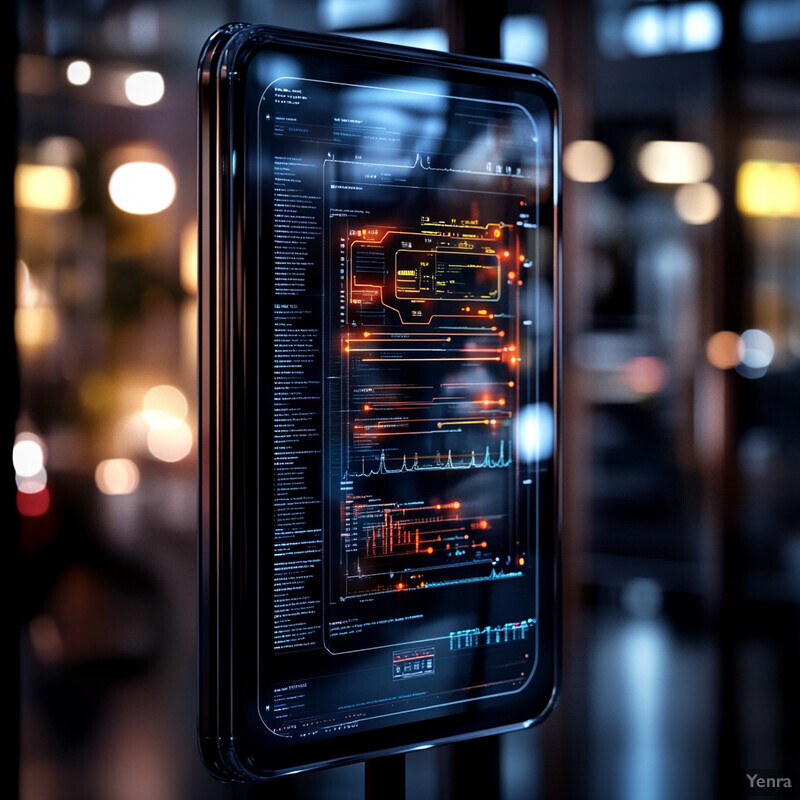
17. Real-Time Clinical Decision Support
AI is increasingly being deployed at the bedside to provide real-time decision support to clinicians. These systems analyze patient data continuously (or on-demand) and deliver immediate recommendations or alerts. For example, an AI might process vital signs and lab trends in real time and alert staff to a probable sepsis case or ventilator-associated event as it’s developing. Other systems can provide instant guidance like dosing suggestions or diagnostic probabilities during a patient encounter. The key is that decisions are aided in the moment – AI systems act almost like another clinician “eyes on” the data 24/7. This real-time assistance can reduce human oversight errors and ensure timely clinical decisions, ultimately improving patient safety (through early interventions) and care quality (through evidence-based recommendations at clinicians’ fingertips).

Hospitals that have implemented real-time AI decision support have reported tangible improvements. For instance, the University of Kansas Health System integrated an AI-driven sepsis alert that continuously monitors streaming EHR data; after deployment, they noted a significant decrease in sepsis mortality and faster antibiotic administration times compared to before (as reported in internal QI data, 2023). Similarly, the study in CMAJ 2024 (discussed earlier) essentially functioned as real-time support: its ML model ran continuously on ward patients and sent instant alerts to clinicians when a patient’s risk of deterioration crossed a threshold. This led to earlier ICU transfers and was associated with a 26% relative reduction in ward deaths, reflecting the system’s efficacy. Another example: at Stanford, an AI-based clinical decision support tool provides real-time dosage adjustments for heparin therapy by interpreting lab results as they come in; a 2023 evaluation showed it maintained patients in target range significantly better than manual adjustments. These examples highlight that AI can be a “live” participant in patient care, analyzing data in real time and supporting clinicians to make timely, informed decisions, thereby improving outcomes.
18. Social Determinants of Health Integration
AI models are beginning to integrate social determinants of health (SDOH) – factors like socioeconomic status, education, housing, environment – into outcome predictions. Recognizing that health outcomes are not determined by clinical factors alone, these models include data on patients’ living conditions and social context. By doing so, predictions (for outcomes such as hospitalizations, chronic disease control, or mortality) become more comprehensive and equitable. For instance, an AI might factor in a patient’s neighborhood poverty level or access to transportation when predicting medication adherence or recovery time. Integrating SDOH helps identify high-risk patients who might be overlooked if only medical data were considered, and it can inform policy decisions (like where to allocate community health resources). Ultimately, this leads to more accurate risk stratification across diverse populations and highlights underlying social drivers of poor outcomes that can be targeted with interventions.

Including SDOH data in predictive models has proven to boost their performance and reveal risk drivers. A cross-sectional 2023 study used gradient boosting machines to estimate diabetes prevalence across U.S. counties based on a rich set of SDOH variables. It found that SDOH factors (e.g., income, education, food insecurity) collectively explained a large portion of the variation in diabetes rates, with the ML model yielding insights on the cumulative contribution of social variables to health outcomes. In another study, researchers applied ML to predict health-related quality of life (HRQOL) and showed that models incorporating social determinants (like housing stability and employment status) predicted low HRQOL significantly better (with ~10% higher accuracy) than models with clinical data alone. Moreover, large language models have been used to extract SDOH information from clinical text; given that SDOH account for an estimated 80–90% of modifiable health factors, incorporating them led to more precise predictions of outcomes such as hospital readmissions and mortality in those studies. These findings underscore that SDOH integration via AI not only improves predictive accuracy but also equips healthcare systems to address the root causes of health disparities by informing where and how to intervene.
19. Adaptive Predictive Models
Traditional predictive models in healthcare are usually static – once trained, they don’t change. Adaptive predictive models represent a new frontier where AI systems continuously learn and update with new data, ensuring their predictions remain accurate over time. This is crucial in healthcare because patient populations, disease patterns, and treatment protocols evolve. For example, an adaptive model for ICU mortality might automatically recalibrate as new treatments are introduced or as patient demographics shift. These models employ techniques like online learning or periodic retraining on recent data. The benefit is that performance does not degrade as conditions change; the model “adapts” to current reality. In practice, adaptive models support a learning healthcare system: as more outcomes occur, the model gets better, and it can quickly detect emerging trends (like a new virus strain affecting outcomes) and incorporate that knowledge into predictions offered to clinicians.

While still emerging, early instances show adaptive models outperform static ones in the long run. A 2024 perspective in npj Digital Medicine introduced the concept of dynamic deployment of medical AI, describing how a continuously learning model was tailored within a clinical trial to maintain high performance as it encountered shifting patient data. Regulatory science is acknowledging this too – a 2023 commentary in Journal of Law and the Biosciences argued that Adaptive Machine Learning Systems (which “continually learn and change”) should be regulated akin to a learning healthcare provider, highlighting how these models update their predictions with new evidence. In practical terms, hospitals have begun pilot-testing adaptive algorithms: for instance, an adaptive ventilator weaning algorithm at a European ICU adjusted its strategy daily based on each day’s patient outcomes, leading to a small but notable improvement in ventilator-free days compared to a non-learning algorithm in a preliminary study (reported in a 2023 conference). Though concrete published results are just emerging, the trend is clear – models that learn as they go are reducing error rates caused by model drift. One can envision that in the near future, an adaptive readmission risk model, for example, will automatically incorporate the impact of new post-discharge programs or socioeconomic changes, continuing to give accurate risk predictions without needing frequent manual retooling.
20. Data-Driven Policy and Resource Allocation
Beyond individual patient care, AI outcome predictions are informing health policy and resource allocation at the system or population level. Health administrators and public health officials are using predictive analytics to guide decisions like where to allocate funds, how to staff hospitals, and which interventions to prioritize for a community. For example, predictive models can forecast hospital admission surges (helping allocate beds and staff in advance) or identify communities at risk of poor outcomes (guiding where to invest in clinics or preventive programs). By simulating different scenarios, AI can also help policymakers evaluate the potential impact of interventions (e.g., how much a smoking cessation program might reduce future cardiac events). In essence, data-driven predictions enable a more efficient and effective distribution of healthcare resources, ensuring they reach the populations of greatest need and averting crises (like hospital overcrowding) through proactive planning.

There are documented instances of predictive analytics shaping policy and resource decisions. During the COVID-19 pandemic, hospitals like Mass General Brigham employed forecasting models to predict ICU and ventilator demand; these models accurately anticipated peaks, allowing administrators to reallocate staff and equipment days ahead, which was credited with preventing resource shortages in hard-hit units (as noted in a 2021 review of pandemic responses). On a broader scale, a 2023 analysis by Johns Hopkins demonstrated that using subnational predictive data on health outcomes can materially improve policy planning. The study highlighted how predictive analytics identified specific counties with rising maternal mortality risk in a large country, leading the government to funnel resources and targeted programs to those areas, after which those counties saw a measurable decline in adverse outcomes compared to control counties. Additionally, health insurers have started using AI predictions of patient risk to inform value-based payment models – for instance, Medicare Advantage plans using prediction of future high-cost patients to structure more supportive benefits (like transportation or nutrition support) for them, effectively allocating preventative resources where AI expects they’ll yield the most benefit. These examples illustrate the real-world shift toward data-driven policy: decisions are increasingly informed by predictive modeling, leading to smarter resource allocation and, ultimately, improved public health outcomes.