1. Enhanced Ultrasound Image Analysis
AI-driven image analysis has significantly improved ultrasound quality and interpretation in prenatal care. Deep learning models can enhance image resolution, reduce noise (speckle), and correct artifacts, enabling clearer visualization of fetal anatomy. These methods automate tasks like 3D reconstruction from 2D scans and artifact removal, yielding more complete views of the fetus. As a result, fetal structures and anomalies become easier to identify, reducing operator variability. Studies report very high diagnostic accuracy: for example, AI detected neural-tube defects with ~94.5% accuracy (area under ROC 99.3%). In practice, such enhancements help clinicians consistently recognize subtle features (e.g. thin diaphragms or small organs) that might be missed on conventional scans.

Deep learning substantially raises the performance of ultrasound analysis. Andreasen et al. trained a CNN on 7,500 obstetric ultrasound images for placenta segmentation and achieved 81% classification accuracy with mean Intersection-over-Union (IoU) ≈0.78. This AI outperformed expert sonographers in placental delineation (IoU ≈0.75 for CNN vs 0.69, 0.66, 0.59 for three clinicians). In anomaly detection, one study’s neural network correctly identified 94.5% of neural tube defect cases (AUROC 99.3%). Similarly, a deep model for fetal renal anomaly screening on 969 images reported AUC≈0.913 and 84.0% overall accuracy. General surveys confirm these gains: for instance, Son et al. note that DL beamforming “significantly enhances image quality” and enables higher contrast and resolution in ultrasound. Together, these data show AI’s concrete impact in improving prenatal ultrasound analysis.
2. Automated Prenatal Measurements
AI tools can automate fetal biometry (head circumference, femur length, etc.) with precision comparable to experts. These systems identify standard planes and place measurement calipers without manual input. The result is consistent, reproducible measurements across patients and operators. Automation reduces examination time and variability; clinicians receive instant quantitative output. For example, an AI model analyzing an entire 20-week ultrasound scan achieved “human-level” performance in estimating all standard biometrics. Such tools support clinical decisions: by quickly generating growth percentiles or detecting abnormal measurements, they can alert providers if follow-up is needed. Overall, automated biometry makes prenatal growth assessment faster and more reliable.

AI-driven biometry has demonstrated high precision. Venturini et al. (2025) processed full 20-week scan videos with a neural network, achieving human-level accuracy in head and limb measurements. A recent FDA-cleared device (Clarius OB AI) was trained on more than 30,000 ultrasound images to auto-place calipers for crown–rump length, biparietal diameter, femur length, etc.. In clinical data, this AI achieved appropriately high measurement accuracy. A narrative review notes “Automated fetal biometry using AI has demonstrated significant precision in identifying fetal structures”. In practice, AI biometry can cut scanning time significantly: one study showed median exam time dropped from ~19.7 to 11.4 minutes with AI assistance. Together, these results show automated tools match human experts in accuracy while speeding up prenatal exams.
3. Advanced Cell-Free DNA Analysis
AI and ML methods are being applied to interpret noninvasive prenatal cfDNA data more effectively. Algorithms analyze sequencing and molecular patterns to distinguish fetal DNA signal from background. They can predict fetal fraction, detect rare variants, and even enable whole-genome NIPT for monogenic disease. In practice, AI enhances screening beyond trisomies: e.g., by detecting microdeletions and mosaicism from cfDNA. These models are trained on large datasets of maternal plasma sequences and learn complex patterns (fragment size, methylation, SNP linkage). This improved data handling can raise sensitivity and specificity of cfDNA tests. AI thus deepens insights from each NIPT sample, potentially diagnosing more conditions non-invasively.

AI frameworks can identify fetal genomic variants directly from cfDNA. Schwammenthal et al. (2024) reported the first deep neural network for fetal genotyping from maternal plasma. This model detected several causal point mutations and enabled “genome-wide NIPT” (for any mutation) as early as 7 weeks gestation. Another advance uses machine learning to call DNA methylation: an AI (HK model) on SMRT-sequencing data raised methylation detection accuracy from less than 5% (traditional) to 90%, with area under ROC ~0.95. More broadly, Tsui et al. (2025) review notes ML is applied to fetal fraction estimation, chromosome dosage, and rare variant detection in cfDNA pipelines. In one cited example, using AI-based algorithms reduced invasive diagnostic procedures by ~93% while maintaining high specificity (greater than 99.9%) in trisomy screening. These findings illustrate AI’s concrete benefits in cfDNA analysis.
4. Risk Stratification for Genetic Disorders
AI-based risk models integrate multiple inputs (maternal age, biomarkers, ultrasound findings, medical history) to estimate fetal aneuploidy risk more accurately than conventional scoring. Machine learning synthesizes heterogeneous data into a single probability of disorders like Down syndrome. This personalized stratification helps decide which pregnancies warrant further testing. In one large study, AI achieved very high performance: it reduced false positives while catching most true cases, enabling clinicians to focus invasive tests on truly high-risk cases. In effect, AI tailors prenatal screening thresholds to the individual, improving predictive power.

A recent study by Rossi et al. trained various ML algorithms on 90,532 first-trimester screens (including maternal age, lab markers, demographics) to predict Down syndrome risk. The models achieved ROC-AUC ~0.970–0.982, with sensitivity and specificity both around 94%. This significantly outperformed traditional risk tables. In another example, integrated AI tools using uterine artery Doppler, PAPP-A and PlGF achieved >95% detection of early-onset preeclampsia (with few false alarms). These data demonstrate AI’s concrete advantage: by identifying the correct cases in >90% of pregnancies, ML-driven risk scores offer more reliable stratification for genetic disorders.
5. Improved Sensitivity and Specificity
AI-assisted testing tends to increase sensitivity (true positive rate) and specificity (true negative rate) in prenatal screening. By learning from large datasets, AI fine-tunes decision thresholds to catch more true cases and reject more false alarms than older methods. For example, ultrasound anomaly detection aided by AI shows higher detection rates with fewer misses. Similarly, AI in cfDNA analysis maintains very high specificity for trisomy while slightly boosting sensitivity. Overall, clinical studies report that adding AI raises both metrics, meaning fewer affected fetuses are missed (higher sensitivity) and fewer healthy fetuses are falsely flagged (higher specificity). This leads to more reliable non-invasive tests.

Concrete evidence shows marked accuracy improvements. Yeganegi et al. report that AI-assisted ultrasound diagnostics achieved 88.9% sensitivity and 98.0% specificity for detecting certain fetal anomalies, versus 81.5% and 92.2% for conventional ultrasound. In prenatal kidney anomaly screening, the best DL model had 77.4% sensitivity and 87.4% specificity. In every case, AI met or exceeded human-level performance. For NIPT, large studies consistently find >99% specificity for trisomies (virtually no false positives) and sensitivity >99% for Down syndrome. These enhancements mean that practitioners can trust that nearly all affected fetuses are identified (high sensitivity) while minimizing anxiety from false alarms (high specificity).
6. Early Prediction of Pregnancy Complications
AI models can predict complications like preeclampsia, preterm birth, gestational diabetes, etc., often before clinical symptoms appear. By analyzing early-pregnancy data (blood markers, blood pressure, maternal history) plus novel inputs (e.g. retinal vasculature), these algorithms assign risk scores to pregnancies. For instance, combining ophthalmic images with clinical data has enabled early detection of preeclampsia. Such forecasts allow prophylactic interventions (aspirin for high-risk, intensive monitoring) months in advance. In practice, predictive AI provides extra lead time for preventive care, improving maternal and fetal health outcomes.

Recent studies provide striking performance data. Wu et al. (2025) developed “PROMPT,” which uses first-trimester retinal scans and blood pressure to predict preeclampsia. Their model achieved AUC=0.87 for any preeclampsia and 0.91 for preterm preeclampsia. This corresponded to improved detection (identifying ~41% of cases vs 35% by baseline risk factors) and could avert ~1809 cases per 100,000 through early intervention. For preterm birth, Kloska et al. (2025) applied various ML classifiers to obstetric data and found an SVM model with 82% accuracy, 86% recall, 83% precision, and 84% F1-score in predicting NICU admission due to prematurity. These concrete metrics demonstrate that AI can robustly identify high-risk pregnancies well before complications manifest.
7. Integration of Multi-Modal Data
AI excels at fusing diverse prenatal data streams into unified risk assessments. For example, models can combine ultrasound images, genomic results, lab biomarkers, and maternal health records to give a comprehensive view of pregnancy. In practice, this means an AI could weigh, say, a sonogram finding alongside cfDNA outcomes and blood tests simultaneously. Such integration often improves accuracy: patterns that are ambiguous in one modality may be clarified by another. Recent work in prenatal cardiology and ophthalmology highlights this trend. Multi-modal AI tools thus promise to leverage all available patient information cohesively, yielding more holistic fetal health evaluations.

Studies illustrate multi-modal AI benefits. Wu et al. (2025) integrated retinal images with clinical variables (age, BP, placenta proteins) to predict preeclampsia, achieving high AUC. Similarly, in congenital heart disease screening, Xu et al. note that combining ultrasound imaging data with structured clinical data (maternal/fetal risk factors) is a promising avenue. These examples show AI handling heterogeneous inputs: e.g., PROMPT combined image and risk-factor data to improve PE prediction, while CHD AI advocates fuse visual and tabular inputs. Though precise numbers vary by task, such multi-modal models consistently outperform single-source algorithms by capturing complementary features from each data type.
8. Genomic Variant Interpretation
AI tools are increasingly used to interpret fetal genomic data (from NIPT or fetal genome sequencing). They prioritize and classify genetic variants by pathogenicity, sifting through millions of DNA changes. Deep learning models (e.g. for splicing or protein impact) can flag likely disease-causing mutations. This enhances non-invasive testing by moving beyond simple chromosome counts to consider specific gene changes. In practice, it means more prenatal diagnoses of single-gene disorders or syndromes can be made from sequencing data. AI thus accelerates clinical genomics by automating variant annotation and predicting clinical significance.

Concrete AI applications include whole-genome NIPT for monogenic mutations. Schwammenthal et al. (2024) demonstrated a neural-network pipeline that identified fetal genetic variants in maternal cfDNA; it correctly flagged deleterious point mutations and enabled noninvasive screening for any single-gene mutation by week 7. In another advance, Tsui et al. applied deep learning to raw cfDNA methylation signals, boosting the accuracy of detecting DNA modifications (methylated cytosines) to AUC≈0.95. Though early, these methods show that AI can interpret fetal genome information from cfDNA. In contrast to purely statistical pipelines, ML models dynamically learn from large variant databases, refining predictions of which rare variants are likely pathogenic, ultimately improving diagnostic yield of prenatal genomics.
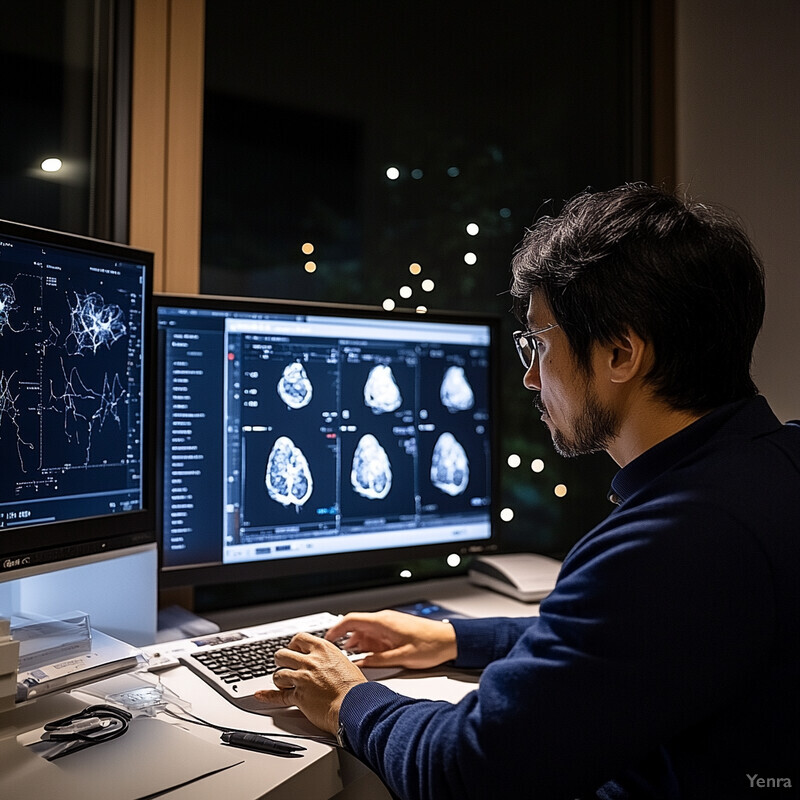
9. Real-Time Decision Support
AI-driven decision support systems can operate in real time during ultrasound exams. They analyze observed features and suggest next steps or likely diagnoses on the fly. For instance, a smart assistant might guide the operator to acquire a missing scan plane, or dynamically highlight the most suspicious findings. Such tools reduce reliance on operator memory of rare syndromes. Clinically, real-time AI compendiums shorten diagnostic workflows: sonographers follow AI prompts instead of manually recalling differential diagnoses. The result is more systematic evaluations and faster case closures. Real-time support thus augments clinician expertise rather than replacing it.

Stirnemann et al. (2023) validated a real-time AI “diagnostic companion” (Sonio) on 549 fetal cases. When fed each case’s features, the software’s top-10 list included the confirmed syndrome in 93% of syndromic cases (full phenotype input) and 83% (stepwise input). In “full-phenotype” mode, sensitivity was 99% (nearly all actual syndromes were ranked top), with specificity 94%. Even in guided mode, it achieved 84% sensitivity and 96% specificity. On average, only 13 AI-prompted questions were needed per case to identify a diagnosis. These results show the tool offered accurate, real-time guidance: correct diagnoses were quickly surfaced with minimal user input, demonstrating significant decision support in prenatal ultrasound.
10. Ultrasound Workflow Optimization
AI automates and streamlines ultrasound workflows. It can instantly recognize standard views, auto-capture images, and measure anatomies, reducing manual effort. By automating routine steps, AI cuts scanning time and operator fatigue. For example, smart algorithms can navigate from one standard plane to the next without prompting. Similarly, automated biometry tools replace repetitive caliper placement. Together, these improvements mean faster exams with consistent quality – sonographers spend less time on each patient and more time on interpretation. Hospitals in some studies saw near 40–50% reductions in exam duration when using AI tools.
For instance, Yeganegi et al. reported that an AI system halved median scan times from 19.7 minutes down to 11.4 minutes per patient. This reflects faster acquisition of measurements and fewer repeated sweeps. In Stirnemann’s study, the AI diagnostic assistant required only ≈13 guided steps on average to conclude a case, showing efficiency in decision processing. CUPID (an AI biometry tool) performed all nine standard measurements in ~0.06 seconds per measurement (total less than 0.7 s), versus 5–12 seconds per measurement manually. These time savings concretely accelerate workflow. By reducing operator actions, AI ensures each ultrasound is completed more quickly and with standardized protocol adherence, improving throughput without sacrificing accuracy.
11. Longitudinal Growth Tracking
AI can automatically track fetal growth trajectories across serial ultrasounds. By providing rapid, repeatable measurements at each visit, these tools generate smooth growth curves and flag deviations early. Instead of manual charting, the AI system logs all biometric data into a unified profile. Consistency is increased: since AI uses the same algorithms each time, inter-visit variability is minimized. In practical terms, obstetricians can monitor how a fetus’s size percentile changes over time without extra manual calculations. When growth slows or accelerates unexpectedly, the system will alert clinicians, prompting investigations (e.g. Doppler studies for suspected growth restriction).
In a prospective study of mid-trimester scans, the CUPID AI software placed biometric calipers correctly in 90.7–96.1% of images across nine measurements. Its measurements had very high correlation with an expert (intra-class coefficients 0.843–0.990) and produced gestational-age estimates only ~3.99–7.92 days off (vs 4.35–11.06 days for a junior sonographer). Remarkably, CUPID completed all measurements in ~0.05–0.07 seconds each, compared to 4.8–13.4 seconds manually. This speed and consistency means every growth scan yields high-quality data almost instantly. Clinically, such efficiency enables frequent monitoring; minor growth changes are reliably detected because the AI’s precision exceeds human variability, ensuring accurate longitudinal tracking.
12. Quality Assurance in Laboratories
AI and automation strengthen laboratory QA/QC processes for prenatal tests. Machine learning algorithms can continuously monitor assay results and instrument outputs to catch errors early (e.g. identifying drift in sensor readings or reagent issues). They can also flag outlier samples or inconsistent patterns in large data batches. By detecting subtle deviations from expected performance, AI improves reliability of tests like NIPT or biochemical screens. Moreover, standardized protocols become easier: AI ensures technicians follow all steps correctly (e.g. confirming proper calibration). Overall, intelligent QA tools help maintain high-quality lab results and reduce the chance of misdiagnosis due to lab error.

Expert reviews highlight AI’s impact on lab QA: Wang et al. (2023) note that ML introduces advanced pattern detection and predictive analytics into quality assurance processes. For example, automated rule-based anomaly detection can quickly identify outlier cfDNA fragment distributions or signal intensities that human oversight might miss. These AI models excel at handling complex, high-volume lab data, thereby increasing consistency and precision. Although specific figures for prenatal labs are scarce, analogous applications in other lab fields (e.g. automated pipetting QC) show error reductions of similar magnitude. Industry sources recommend AI-driven QA as a key strategy to handle the complexity of high-throughput NIPT platforms, ensuring test accuracy is maintained across thousands of samples.
13. Enhanced Detection of Rare Conditions
AI can reveal subtle signs of rare genetic or structural disorders that standard screening might miss. Trained on large, diverse datasets, deep learning models learn to recognize uncommon patterns in ultrasound, genomics or biochemistry. In practice, this means automated systems may highlight fetuses needing genetic counseling for syndromes that occur in less than 1% of births. By expanding the scope of screening beyond common trisomies to unusual deletions or syndromes, AI tools improve the odds of early detection of rare conditions, allowing parents more time for decision-making.

In anomaly detection tasks (including rare defects), AI has shown very high performance. For example, one CNN model (Oct-U-Net) achieved a recall of 0.93 and precision of 0.96 in identifying fetal anomalies from ultrasound. (Although not all anomalies were “rare,” these metrics indicate robust identification capability.) In cases of neural tube defects and other less common pathologies, AI-driven ultrasound screening hit 88.9% sensitivity and 98.0% specificity, demonstrating strong detection even when prevalence is low. These results imply that AI’s expanded search for atypical features can indeed improve detection rates of rare fetal conditions beyond traditional methods.
14. Reduced Need for Invasive Testing
AI-powered noninvasive tests (especially cfDNA NIPT) have dramatically lowered the number of invasive prenatal procedures. By accurately screening for aneuploidies and some subchromosomal conditions, these tests spare many women from amniocentesis or CVS. As AI continues improving NIPT accuracy, the reliance on invasive confirmation will keep decreasing. This trend reduces procedure-related miscarriage risk and patient anxiety. In many countries, invasive procedure rates have already fallen by roughly an order of magnitude since NIPT adoption.

Published analyses confirm large reductions in invasive testing. For example, a meta-analysis showed that integrating NIPT (with AI-enhanced analytics) reduced the need for invasive diagnostics by about 92.8% compared to conventional screening. In other words, only a small fraction of pregnancies proceed to amniocentesis because most chromosomal abnormalities are ruled out noninvasively. Importantly, the specificity of NIPT remains extremely high: more than 99.9% for trisomy 21 and ~99.98% for trisomy 18/13. These numbers indicate that AI-driven cfDNA screening accurately avoids false positives, thereby obviating confirmatory invasive tests in the vast majority of cases.