1. Enhanced Precision
AI-powered surgical robots greatly enhance the precision of operative maneuvers. These systems can execute delicate tasks with sub-millimeter accuracy, far steadier than a human hand. By analyzing sensor feedback and patient-specific data, AI algorithms adjust instrument motion to avoid even slight deviations. This heightened precision is crucial in delicate procedures (such as neurosurgery or ophthalmology) where millimeters can determine outcomes. Improved precision means less inadvertent damage to healthy tissue, which can lead to faster healing and better functional results for patients.
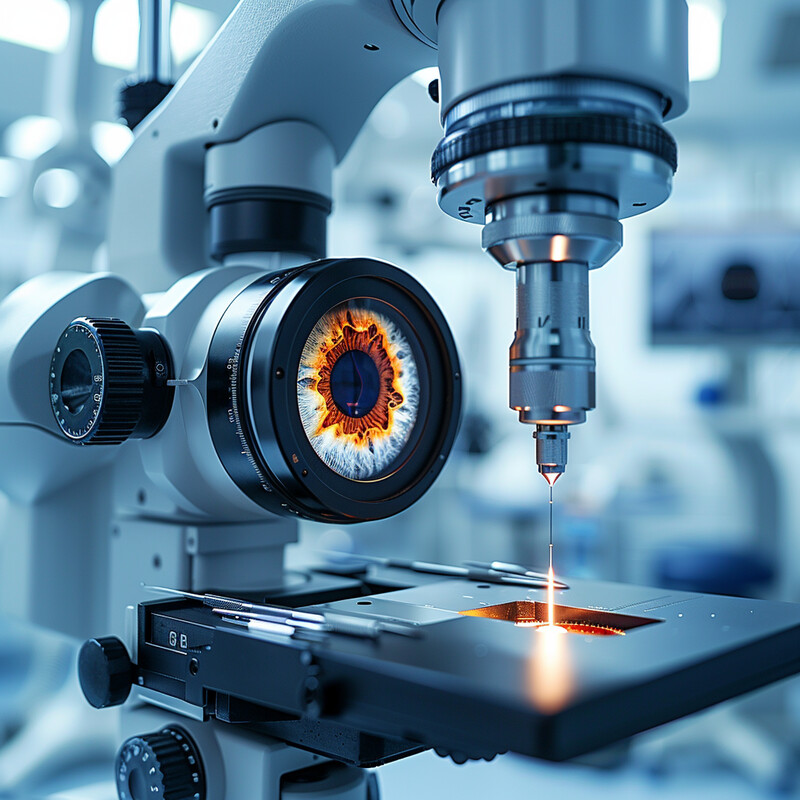
AI integration in surgical robotics has been shown to improve the accuracy of instrument positioning and associated outcomes. For example, a recent meta-analysis of knee replacement surgeries found that robot-assisted procedures achieved more precise implant alignment, which translated to a 14% shorter hospital length of stay for patients compared to traditional methods. By enabling such exact placement of surgical tools and implants, AI-guided robots reduce postoperative pain and expedite recovery, underscoring the tangible patient benefits of enhanced precision.
2. Real-time Decision Making
AI enables surgical robots to make intelligent decisions on the fly during operations. By processing live data from cameras, sensors, and patient monitors, an AI-driven system can recognize unexpected events—such as a sudden bleed or tissue abnormality—and adjust its strategy instantly. This real-time adaptability means the robot can change course or alert the surgical team within seconds, something that traditionally relies on human reaction time. AI algorithms can also continuously optimize movements during a procedure, ensuring the surgical plan is dynamically refined for the best outcome. Ultimately, real-time decision support enhances the surgeon’s ability to respond to intraoperative changes, improving safety and efficacy in unpredictable surgical environments.
Advanced AI systems are already demonstrating remarkable real-time decision capabilities in surgery. In 2024, researchers introduced an AI model called FastGlioma that can analyze surgical data in seconds during brain tumor operations. This system was able to detect residual cancerous tissue with about 92% accuracy in just 10 seconds, dramatically outperforming standard methods. In a comparative study, the AI’s real-time analysis missed high-risk tumor remnants in only 3.8% of cases, versus a nearly 25% miss rate using conventional intraoperative techniques. By immediately identifying remaining tumor tissue that surgeons might otherwise overlook, AI-driven decision support like this can guide surgeons to remove all dangerous tissue on the spot, illustrating how real-time AI interventions can directly improve surgical completeness and patient outcomes.
3. Preoperative Planning
AI significantly improves preoperative planning by tailoring surgical strategies to each patient’s unique anatomy and condition. Before a surgery, AI algorithms can analyze medical images (like CT/MRI scans) and patient data to identify the optimal surgical approach. This includes determining the safest incision sites, ideal pathways to avoid vital structures, and anticipating potential challenges (such as anatomical variations or risk of complications). By simulating different scenarios, AI can help surgeons “rehearse” the operation and refine the plan for maximum efficiency and safety. The result is a customized surgical roadmap that can shorten operative time and reduce intraoperative surprises. Overall, AI-driven planning leads to more predictable surgeries and better alignment between the planned and actual procedure.

AI-driven preoperative planning tools have been shown to improve risk prediction and operative efficiency. A recent systematic review of general surgery outcomes reported that incorporating AI into the planning phase improved the accuracy of predicting postoperative complications by about 25% compared to traditional risk assessments. For instance, machine learning models analyzing patient history and imaging could foresee potential issues (like likelihood of infection or bleeding) with significantly greater precision, allowing surgeons to proactively adjust their game plan. These same AI systems also helped reduce average surgical duration – one analysis noted an average reduction of 30 minutes in operating time for complex cases when AI guidance was used in planning. By better stratifying patient risk and streamlining surgical strategy, AI-based preoperative planning contributes to safer surgeries and smoother recoveries.
4. Minimally Invasive Techniques
AI is a driving force behind the expansion of minimally invasive surgical techniques. By guiding robotic arms with exceptional precision, AI allows surgeons to operate through very small incisions or natural orifices, as opposed to large open cuts. These minimally invasive (often laparoscopic or endoscopic) approaches benefit patients through reduced trauma: smaller incisions mean less blood loss, lower infection risk, and decreased postoperative pain. Patients undergoing AI-assisted minimally invasive surgeries typically experience faster recovery and shorter hospital stays because their bodies endure less stress. In addition, AI helps overcome some challenges of minimally invasive surgery, such as limited visibility or instrument maneuverability, by enhancing imaging and steadiness. This means even complex surgeries (in cardiothoracic, colorectal, urologic, etc.) can increasingly be done in a minimally invasive manner with the aid of AI, improving patient comfort and outcomes.

The adoption of AI-enabled robotic systems has vastly increased the prevalence of minimally invasive surgery across many fields. In the United States, for example, over 85% of all radical prostatectomies are now performed with robot-assisted, minimally invasive techniques. This rapid uptake—from virtually 0% two decades ago to the dominant technique today—reflects the proven benefits of smaller incisions and enhanced precision for patients. Studies consistently find that patients who undergo robotic minimally invasive procedures have shorter hospital stays (for instance, prostate surgery patients average ~1.6 days with robotics vs 2+ days with open surgery) and report lower pain levels postoperatively. The overwhelmingly high utilization of AI-guided minimally invasive surgery in prostate cancer (and similarly in gynecologic and other surgeries) underscores how AI is enabling safer surgeries with quicker recoveries on a national and global scale.
5. 3D Visualization
AI synergizes with advanced imaging technologies to provide surgeons with rich 3D visualizations of the operating field. Instead of relying solely on conventional 2D camera views, surgeons can get augmented reality (AR) or three-dimensional reconstructions in real time, thanks to AI image processing. This means critical structures (like blood vessels, nerves, or tumors) can be highlighted and seen in depth, improving the surgeon’s spatial awareness. AI can fuse data from CT/MRI scans with live camera feeds, creating a virtual 3D map that overlays onto the patient during surgery. Such enhanced visualization is especially beneficial in complex anatomy or minimally invasive settings, where direct line-of-sight is limited. By giving surgeons “X-ray vision” and depth perception during procedures, AI-driven 3D visualization improves accuracy of instrument placement and helps avoid inadvertent damage, thereby making surgeries safer and more effective.

The benefits of AI-enhanced 3D visualization are evidenced by improved surgical accuracy metrics. A 2024 study at Hospital for Special Surgery (HSS) compared traditional robotic navigation to a new AI-assisted augmented reality system for guiding spine surgery. The results showed that both approaches achieved extremely high precision in pedicle screw placement – 99.6% of screws placed with robotic navigation and 98.7% with the AR system were rated in optimal positions (Grade A or B). Notably, over 92% of all screws achieved the top-tier Grade A accuracy in the study, underscoring how 3D visualization tools (whether via robotics or AR) can virtually eliminate placement errors. These findings highlight that AI-driven 3D guidance systems provide surgeons with superior visual context, enabling near-perfect accuracy in executing complex tasks like spinal hardware placement. Such precision ultimately translates to better patient outcomes, as proper screw placement is critical for safety and stability in spine surgeries.
6. Skill Transfer and Training
AI is revolutionizing surgical training by capturing expert techniques and disseminating them to others – both human trainees and other robots. Through machine learning, AI systems can analyze countless hours of expert surgeons’ movements (from videos or sensor data) to distill what makes a technique successful. These insights can then be used in surgical simulators or robotic controllers to teach the same skills. For human surgeons, AI-powered training platforms provide real-time feedback on performance, identifying errors or suboptimal moves that a trainee can correct immediately. This creates a personalized learning experience that was not possible with traditional apprenticeship alone. AI can also enable “virtual proctors,” where trainees practice on simulators and an AI coach provides guidance as effectively as a human mentor. Moreover, once a procedure is mastered by one robot (or through an AI algorithm), that knowledge can be transferred to other autonomous robotic systems, standardizing high-level surgical skills across the board. The net effect is faster, more consistent training and the globalization of expert-level surgical techniques.

Early studies show that AI-driven training tools can equal or even surpass human instruction in teaching surgical skills. In a 2024 randomized trial, nearly 100 surgical trainees were taught a complex simulated task (brain tumor removal technique) with different teaching methods: one group received real-time AI feedback, another had traditional in-person expert coaching, and a control group had no real-time guidance. The outcome was striking – the group trained with real-time AI feedback performed significantly better than even the group taught by human experts, as measured by objective surgical skill scores. The AI-trained students achieved proficiency scores on par with those receiving one-on-one expert instruction (with no significant difference in standard ratings between the two). This suggests that an AI “mentor” can replicate the nuanced feedback of an experienced surgeon and do so consistently for every trainee. Separately, AI has also enabled surgical robots to learn directly from experts; for instance, a robotic system trained on videos of expert surgeons was able to tie knots and suture with skill comparable to a human surgeon, even correcting its own errors. These advancements illustrate AI’s powerful role in accelerating skill transfer and ensuring that surgical excellence can be taught and reproduced at scale.
7. Postoperative Monitoring and Care
AI extends the benefits of surgical robotics into the postoperative phase by actively monitoring patients and predicting complications before they fully develop. After surgery, patients can be outfitted with smart sensors and their vital signs, lab results, and even wound images can be continuously analyzed by AI systems. These systems are trained to detect early warning signs of issues like infection, bleeding, or poor healing – often hours or days before they would become obvious to clinicians. If a potential complication is detected, the AI can alert healthcare providers or even suggest an intervention (for example, starting antibiotics at the first hint of infection). Additionally, AI chatbots can engage with patients after discharge, answering questions about their recovery and triaging symptoms, which improves patient reassurance and reduces unnecessary hospital visits. By personalizing post-op surveillance (essentially giving each patient an automated “digital nurse” that never sleeps), AI helps ensure any problem is caught and addressed as early as possible, thereby improving recovery outcomes and reducing readmission rates.

AI-driven postoperative monitoring has demonstrated the ability to both maintain high-quality care and drastically reduce the workload on healthcare staff. A 2025 study in npj Digital Medicine tested an AI system for remote wound monitoring after gastrointestinal surgeries. The AI model analyzed patient-reported symptoms and wound photographs to predict surgical site infections within 48 hours of onset. Remarkably, its accuracy was on par with experienced clinicians – the AI’s performance in predicting confirmed infections (area-under-curve ~0.76) was essentially equivalent to that of human providers (AUC ~0.78). Moreover, by automating data review, the system could cut down the time nurses and doctors spent on routine post-op surveillance by an estimated 80% (reducing staff input from ~51 hours to 9 hours per week) without compromising diagnostic accuracy. This means an AI can reliably watch over recovering patients and flag issues, vastly easing the burden on clinical staff. In another example, post-surgical patient chatbots have been trialed – one obstetrics study reported 96% patient satisfaction with an AI chatbot answering their questions after surgery, indicating that patients are receptive to AI-based follow-up care as an adjunct to their providers. These findings show that AI can play a pivotal role in postoperative care: catching complications early (with predictive analytics) and augmenting the care team in monitoring and guiding patients during recovery.
8. Error Reduction
AI has a profound ability to reduce human error in surgery by learning from large datasets of surgical performance and outcomes. Modern surgical robots equipped with AI continuously collect data from each procedure – every motion, force applied, and event – and use it to refine their algorithms. Through machine learning, the system can recognize patterns that lead to errors or complications (for instance, a certain hand movement that risks cutting tissue at the wrong angle) and adjust to avoid them. AI can also provide real-time prompts or safety checks; for example, warning a surgeon if they are about to operate on the wrong anatomical site or automatically pausing if an unsafe condition is detected. Over time, as the AI gets “smarter” with more experience, the frequency of errors like inadvertent cuts, misplacements of instruments, or lapses in following best practices diminishes. Furthermore, AI doesn’t get fatigued or distracted, so it can maintain a high level of vigilance throughout long surgeries, serving as a consistent safety net. By combining the vigilance and learning capability of AI with the skill of surgeons, the overall rate of surgical errors can be driven down significantly, improving patient safety.

Studies are beginning to quantify how AI assistance leads to fewer surgical mistakes. In a 2025 review that aggregated outcomes from over 12,000 surgical cases, researchers found that surgeries utilizing AI guidance had an 18% lower rate of intraoperative technical errors compared to standard surgeries. These errors include issues like unintended tissue injury or incorrect instrument usage, and their reduction was attributed to AI’s ability to provide real-time corrective feedback and precision control. Another analysis noted that AI-assisted procedures showed more consistent adherence to optimal surgical technique, resulting in measurably fewer complications related to human error. In practical terms, this means if a certain surgical step has historically caused, say, 1 in 5 surgeons to make a slight misstep, the AI can coach that rate down to near 1 in 6 or better – a meaningful improvement when scaled to thousands of operations. As AI systems continue to learn and surgeons become more adept at working with these “co-pilots,” the expectation is that preventable surgical errors (such as wrong-site incisions or accidental instrument slips) will keep trending downward, making surgery safer year by year.
9. Patient-Specific Instrumentation
AI is enabling the design and production of surgical instruments and implants that are custom-tailored to the individual patient. Traditionally, surgeons use standardized tools and off-the-shelf implants, which may not perfectly fit every patient’s anatomy. Now, with AI-driven analysis of patient scans (like 3D imaging of a bone or organ), bespoke surgical guides or implants can be crafted—for example, 3D-printed jigs that match a patient’s bone geometry to guide drill holes with pinpoint accuracy, or custom joint implants that align exactly to a patient’s anatomy. AI algorithms can optimize these designs, ensuring structural integrity and ideal fit, often more efficiently than human designers. This patient-specific approach improves surgical outcomes: implants fit better and thus last longer, and instruments that conform to patient anatomy allow surgeons to perform procedures more easily and safely. It also reduces intraoperative adjustments; if you have a perfectly pre-fit implant or guide, the surgery tends to proceed more quickly and with fewer errors. In essence, AI is helping move surgery away from a one-size-fits-all model toward truly personalized intervention tools.
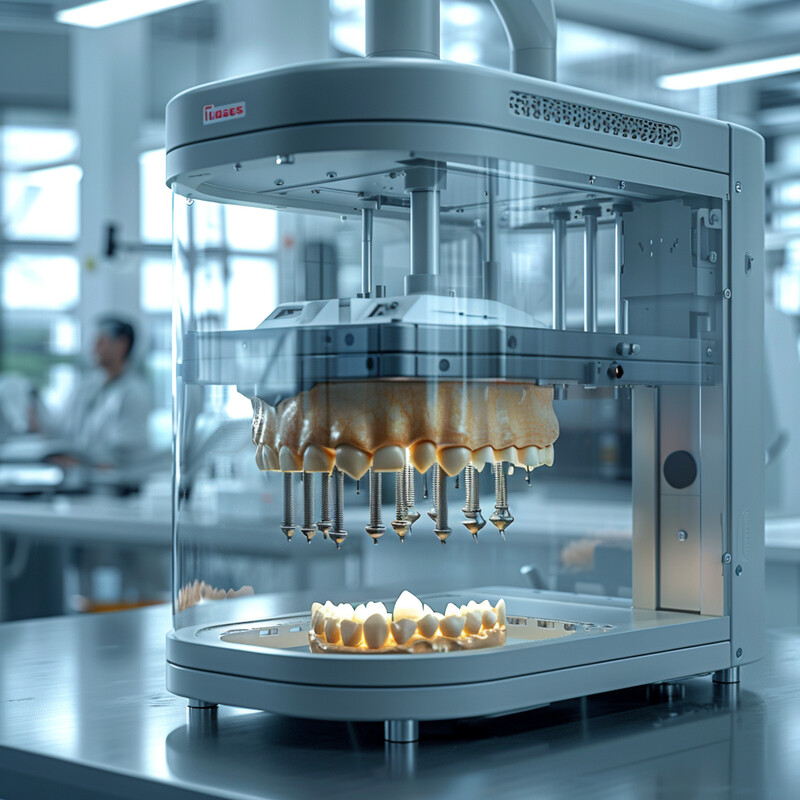
The impact of AI in patient-specific instrumentation is reflected in the growing adoption of customized surgical solutions and improved patient outcomes. In orthopedic surgery, for instance, surgeons are increasingly using AI-generated, 3D-printed cutting guides for knee and shoulder replacements that are made for each patient’s anatomy – studies have reported more consistent alignment and fewer outliers in implant placement when such guides are used. On a broader scale, the patient-matched implant market is expanding rapidly: it’s projected to grow at roughly 7% annually from 2024 to 2031, reaching billions in value. This growth is fueled by successful cases such as custom cranial implants for skull reconstruction (which achieve near-perfect fit and have reduced re-operation rates) and patient-specific spinal rods that conform to individual curvature, reducing postoperative discomfort. One notable example is the FDA’s approval (in 2023) of a personalized airway stent crafted with AI planning – it was shown to reduce complications by accommodating the patient’s exact tracheal shape. These trends and data points underscore that AI-driven personalization is not just theoretical: it’s tangibly improving surgeries, and both industry and hospitals are investing heavily in such patient-specific instrument and implant programs.
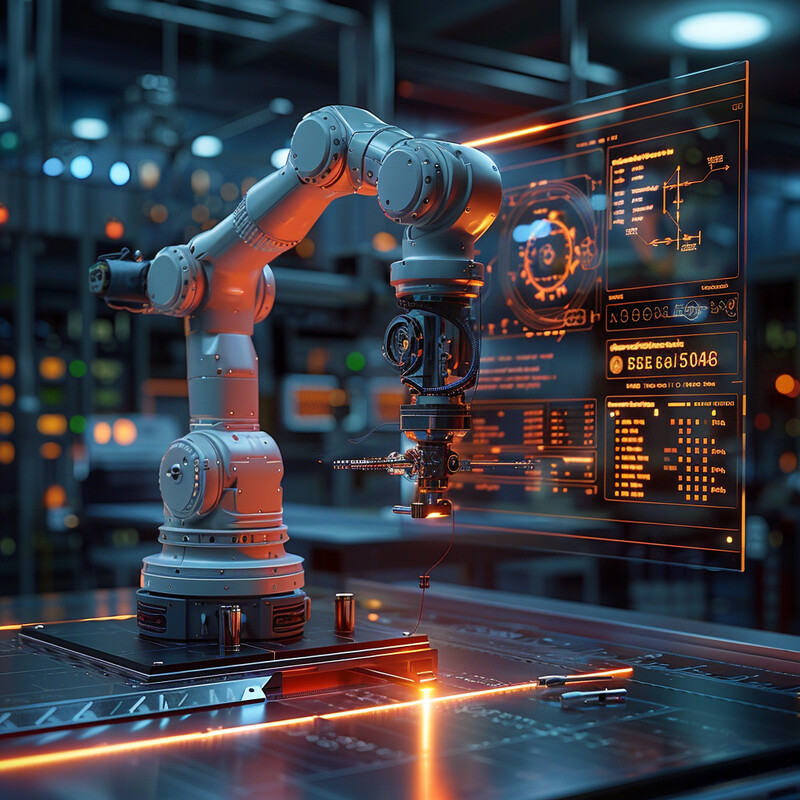
10. Collaborative Robotics
Collaborative robotics in surgery refers to a model where autonomous or semi-autonomous robots work side by side with human surgeons as part of an integrated team. AI makes this collaboration seamless by allowing robots to understand the surgeon’s intentions and complement them. Rather than replacing surgeons, these “co-bots” handle routine or highly precise tasks (like holding instruments steady, suturing, or camera control) while the human focuses on higher-level decisions and nuanced maneuvers. AI enables the robot to adjust in real time to the surgeon’s movements or commands – for example, if a surgeon slightly shifts a patient’s position, the robot can recalibrate its actions accordingly. In the operating room of the near future, you might see an AI-driven robotic assistant suturing one incision while the surgeon closes another, or the robot providing a third hand that exactly follows the lead surgeon’s cues. This teamwork increases overall efficiency (surgeries can be faster when tasks are parallelized) and can enhance safety (the robot can actively prevent the team from making certain mistakes). Collaborative surgical robotics leverages the strengths of both parties: the robot’s precision and tirelessness with the human surgeon’s creativity and judgment. The outcome is a surgical synergy that can tackle complex procedures more effectively than either could alone.
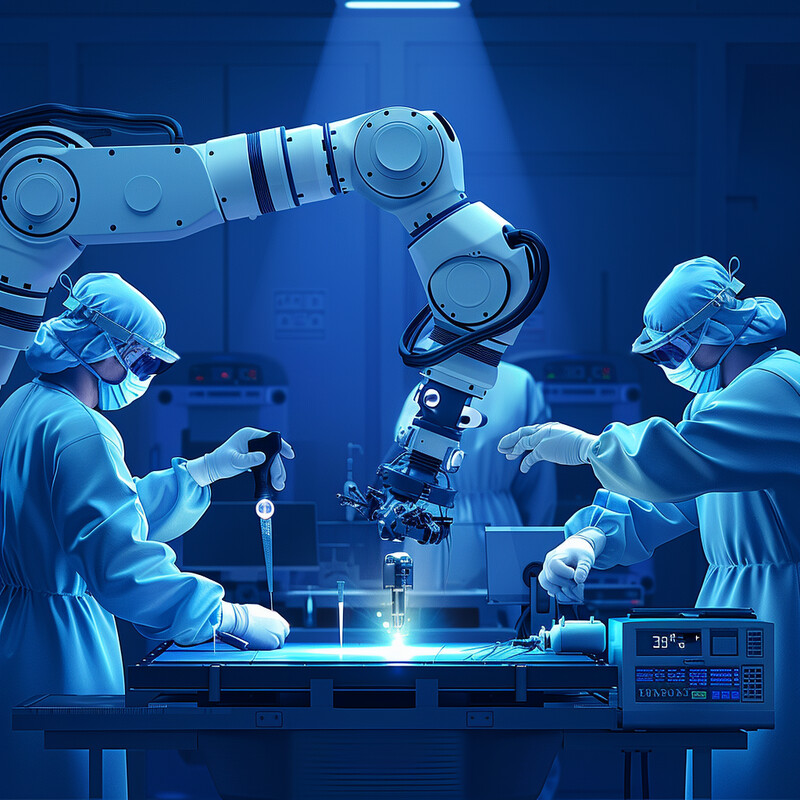
The use of collaborative surgical robots has been accelerating worldwide, highlighting their growing role in operating rooms. By 2023, there were over 7,500 surgical robotic platforms installed globally, and these systems had participated in more than 11 million procedures to date. This proliferation indicates that an increasing number of surgical teams are working with robotic partners on a regular basis. Surveys of surgeons report that these robots, guided by AI, often take over repetitive tasks and can reduce surgeon fatigue, effectively expanding what a surgical team can accomplish in a day. Importantly, collaborative robots are seen as one solution to address workforce shortages – for example, the U.S. is projected to face a shortfall of up to 20,000 surgeons by the mid-2030s. By enhancing each surgeon’s efficiency (one surgeon + one robot can do more than a surgeon alone), AI-assisted co-bots could mitigate some effects of this shortage, ensuring patients still get timely surgeries. The trend is clear: nearly every top hospital now either has a surgical robot or plans to acquire one, not to replace surgeons, but to collaborate with them. With ongoing advancements, these AI-powered teammates are expected to become as common in operating rooms as anesthesia machines – an indispensable part of the surgical team that elevates the capability and performance of human surgeons.